Prosthetic knee: how the operation is performed, who is shown and contraindicated, types of prostheses

Osteoarthritis is almost the most common disease that has a connection with the knee joints. Due to age, cracks appear in the cartilage, the joints wear out. Such processes provoke inflammation, and deformities of joints occur. Diseases of the joints put restrictions on an active lifestyle, constrain movement, deliver pain. Moreover, such manifestations are visible not only during movements, but also in a calm state.
So that the disease of the knee does not become a serious problem, it is important to come to the doctor in the early stages for help. Ignoring the ailments at the initial stages is permission for progression. If, nevertheless, the disease has developed, then the only solution is a prosthetic knee joint, which is made after a scrupulous examination.
Essence of the operation
The essence of the operation of the prosthetic knee joint is surgery, which in time does not take more than 2 hours. The exact implant installation is performed by activating the computer navigation system. Performs manipulation by an orthopedic surgeon.
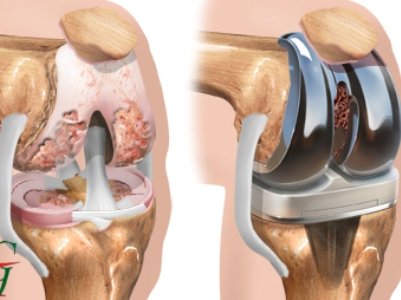
The intervention takes place under general anesthesia, its epidural type can also be used.
Joint replacement may be partial in nature when a prosthesis is placed on certain articular structures, and, if indicated, complete replacement of the joint may be performed.
Before you conduct a planned surgical intervention, an X-ray is required, a general clinical examination of systems and organs is prescribed arthroscopy.
It is also worth noting that the prosthetic knee can be of primary and revision type. In the first case, the operation is carried out for the first time, the second case involves the replacement of a worn endoprosthesis or the development of complications after the previous prosthesis is installed.
Operations can be divided into the following types:
- Endoprosthetics Recreation of damaged elements is performed by introducing artificial prostheses.
- Total prosthetics Intervention, which is carried out only in the case of degenerative type diseases.
- Minimally invasive prosthetics. Compared with the first type of incision has a smaller size.
- Chondroplasty. Surgical intervention involving the elimination of cartilage defects.
Types of endoprostheses
Joint prostheses must necessarily have the following characteristics:
- strength;
- harmlessness;
- excellent survival rate.
Therefore, when choosing an implant, it is important to consider the material from which it was produced. Often used medical and titanium alloys, ceramics, plastics (polyethylene), with high strength.
The most commonly used in surgery are titanium prostheses, as they will last from 15 to 20 years with proper and careful operation. So, prosthetics of the knee joint to the patient will be a quality option that will allow the activity to return. The design of the prosthesis is endowed with metal elements of the tibia, the patella and the femur. For better cushioning, a polyethylene gasket is used. Undoubtedly, the cost of the implant is high, but the result is worth the material costs.
Among the most popular designs are the following types of prostheses:
- Screw prosthesis It is used when there is a need to restore only a small part of the cartilage. It has the appearance of a pin along with a wide cap.
- Associated prosthesis. Used for implantation in case of destruction of a large area of bone tissue. In addition, it is introduced in the event of damage to the ligament apparatus.
- Denture on cement. It has a movable platform, two-way. It helps to get rid of the problem, carrying out revision prosthetics.
- Single Mice. Used to replace a fragment of bone - the upper or lower condyle.
- Interpositional. It is used to restore partially damaged cartilage.
- Special implant. It is made individually depending on the situation of the patient according to the study on computed tomography.
The implantation of a particular type of prosthesis is carried out after discussing the options with the patient and selecting the most appropriate type.
Indications and Prohibitions
Naturally, each patient tries to avoid surgery, resorting to conservative treatment. But sometimes excruciating pain makes it impossible to endure more.
The main indication for surgery is arthrosis, which can be preceded by a number of reasons:
- injuries in which there is a rupture of ligaments, menisci, cartilage, fractures of the articular ends of the tibial and femur bones;
- inflammatory manifestations, for example, gout, rheumatism, arthritis;
- excessive stress on the joints of the knees. This is possible with obesity, in some professional sports;
- congenital defects: dysplasia, deviations of the axes of the lower extremities;
- unsuccessfully performed operations in the area of the knee joints;
- pathologies caused by mechanical stress and permanent injury.
The manifestations of osteoarthritis may indicate the following manifestations:
- Pain in the legs, which occurs during movements, in a relaxed state, in the morning when rising from bed.
- Explicit gait disturbances, difficulty in controlling equilibrium.
- Numbness of the joint, swelling.
These changes are a signal in which the operation is likely to be avoided.
The most important stage after the operation itself is the rehabilitation process, which takes place under the strict supervision of doctors. Adaptation to a new part of the body, especially artificial, for the most part passes as efficiently as possible. Although rejection by the body of a foreign body is not excluded.
Total knee arthroplasty: how the surgery is performed, what complications and rehabilitation are
First of all, arthrosis is capable of provoking the destruction of a knee joint. Late and improper treatment may aggravate the situation. The operation to replace the knee joint is based on the introduction of an artificial implant in place of the damaged one, is partially or completely replaced. Total knee arthroplasty involves complete replacement. The new “knot” in the body is endowed with the same anatomical features as the native. It will allow the patient to overcome pain, begin to actively move and live a full life without any restrictions.
Preparation for surgery

Assigned examinations, including x-rays and tests, are fully tested by a specialist, this is done by the general practitioner, he prescribes the required medications to the patient, which will help to maintain the correct and uninterrupted functioning of the systems and organs during the operation.
Before the operation, the anesthesiologist selects anesthesia depending on the testimony of the patient. On the day of the manipulation is prohibited to eat, drink alcoholic beverages. Allowed a small amount of water.
Before the intervention, total knee arthroplasty involves the imposition of an elastic bandage on a healthy part of the leg. This makes it possible to prevent the formation of blood clots. In addition, a mandatory condition is an emptying of the intestines and bladder.
Surgery and complications
The revision type of joint replacement lasts about 2 hours, the course of the operation with complete total knee joint replacement is as follows:
- the skin surface and soft tissue are cut in layers;
- the affected parts of the bones are removed;
- a joint implant is installed;
- the operative field is cleared of blood, parts of the bone;
- antimicrobial treatment is carried out;
- soft tissue and leather are sutured in layers.
Total knee arthroplasty has a chance of developing complications. These include:
- Damage to the nervous and vascular bundle, which can cause bleeding, disrupt the connection between muscle tissue and the central nervous system.
- Infection of the whole organism by infecting a wound.
- Thrombus formation.
- Pathologies that are associated with the action of anesthesia.
- Implant rejection.
- Disability.
But in most cases, the operation goes well, complications do not arise.
Rehabilitation period
Rehabilitation after surgery is important. So, for the first 24 hours the patient is placed in the intensive care unit. Here are injections of painkillers, necessarily the introduction of antibiotics. In the normal course of rehabilitation, it is possible to sit down for 2 days, minimum physical loads are recommended. Stand allowed for 3 days.
After 10 days, the stitches are removed. In the same period, an extract is made if there are no complications. The next 6 weeks, it is important to use crutches and limit the load on the legs. Also in the rehabilitation period included physiotherapy, therapeutic gymnastics. These activities are aimed at strengthening the tissues around the joints, as well as at restoring the mobility necessary for the implant function.